California is a crucible of innovation and creativity, where new technologies are rapidly transforming health care. In particular, the explosion of digital health tools is spurring a cultural shift in the way that individuals manage their health and well-being, allowing for a more active role, such as the ability to track one’s own health status and use data to guide personal decisions. But how do we ensure that all Californians benefit from this progress?
Ventura County is tackling this problem with a forward-thinking approach to improving outcomes for a population that is often left behind by technology innovations—children and youth in foster care. Last week, the County launched Foster Health Link (FHL), an electronic record for foster parents that includes key health and education information about the kids in their care. Foster Health Link will improve continuity of care for foster youth and their caregivers by moving records from a disorganized and impermanent paper format to an automated, secure system that can be accessed, maintained, and shared electronically. The groundbreaking public-private project, which The Children’s Partnership has supported since its inception, was led by the Ventura County Human Services Agency and received a strong endorsement from the Board of Supervisors last week. The Board described FHL as a huge step forward for foster kids in Ventura County.Antony Brennan, a foster parent from Ventura, said FHL is a time-saver for caregivers who previously had to piece together information about the children in their care from stacks of paper records.
This ambitious project is a shining example of how government agencies can be innovators in the child welfare space and apply technology to find better solutions for the clients they serve. The launch of Foster Health Link is a clear sign of progress for children and youth in foster care in Ventura County, and indeed, a deserving cause for celebration.
Read about Foster Health Link in the Ventura County Star.
Check out Ventura County Foster Health Link.
Learn more about the benefits of care coordination for children and youth in foster care.
Today, I had the opportunity to present to the Little Hoover Commission, an independent state oversight agency, on ways to help ensure children enrolled in Medi-Cal get the dental care they need.
The Commission’s review, requested by Senator Richard Pan and Assemblymember Jim Wood, is in response to a recent audit of the State’s Medi-Cal dental care program that found poor access to care and lack of oversight of the program that put the more than five million children enrolled in the program at higher risk for dental disease.
When children’s oral health is neglected, they needlessly suffer and lose the opportunity to realize their full potential. Poor dental health can disrupt normal childhood development and seriously damage overall health. Children with poor oral health end up in the emergency room, and they miss school due to dental problems.
The audit report and the efforts of the Little Hoover Commission—along with the fact that we now have a state dental director to lead statewide efforts to improve the oral health of California’s residents—provide the impetus and tools to finally make real change and put California on the path to ensuring its children have the optimal oral health care they need to stay healthy and succeed in school and life.
The Children’s Partnership’s recommendations to improve children’s oral health are threefold:
1. Bring Care to Where Children Are. If we are truly committed to the oral health of all children, bringing timely dental care to where they are can make a big difference. The Virtual Dental Home brings care to children in schools, Head Start sites, or other community settings. We were pleased to see the enactment of AB 1174 in 2014, and we hope to see enactment of AB 648 in the near future to continue to expand this cost-effective approach to dental care for children.
2. Invest in Preventive Care for Young Children. Young children enrolled in Medi-Cal receive dental services at disproportionately low rates, even though their needs deserve particular attention. Early preventive dental care results in better oral health as well as overall health and well-being over a lifespan. The State needs to address the needs of young children, which could include raising reimbursement rates for providers who see this population or raising rates for particular services that impact this population, such as preventive services.
3. Make the Most of Our Workforce. We can no longer assume that the dentist is the only provider that can address children’s dental care needs. It takes a team to provide the comprehensive oral health education, care management, and treatment families need. Dental hygienists and assistants are helping to bring care to where children are through the Virtual Dental Home. Community health workers can play a vital role in educating families about the importance of good oral health and how to achieve it, as well as connecting families to services. And home visitors can also play a critical role in getting families off to a good start. California should explore how to adopt and support best practices for expanding outreach, education, and services to improve dental care. Improving the oral health of California’s underserved children is a top priority for The Children’s Partnership, but it will take a coordinated effort of the Administration, the Legislature, and stakeholders to truly make a difference. We look forward to continuing to work with the State to ensure that Medi-Cal’s children—more than half of all of California’s children—have the good oral health they need to be healthy and succeed in life.
Back-to-school time is here, which is the perfect time to help connect children and families with health coverage and care! In fact, this year, schools in California are required to inform families about health coverage opportunities when kids enroll in school. To help schools comply with this new law (AB 2706), The Children’s Partnership’s ALL IN For Health Campaign has a brand new toolkit with everything schools need.
This newly launched Back to School Toolkit has a suite of materials to help schools reach families with easy-to-understand enrollment information. For example, the 2015–2016 School Year Calendar is an exciting new piece for school leaders that lays out a clear roadmap of health coverage outreach activities that fit into the school calendar to help educators schedule out activities. The toolkit also includes the newly released “Are you DACAmented?” flyer that will help schools reach families who have children with DACA status and connect them with health coverage.
As kids’ advocates, The Children’s Partnership has worked since its founding to better the health of children and families throughout California and across the nation. The ALL IN For Health Campaign has been a key part of that mission.
In order to leverage the once-in-a-generation opportunity provided by the Affordable Care Act to extend health coverage to more Californians than ever, we have partnered with the education community. Educators interact with millions of families every day and understand better than anyone that healthy kids make better learners.
We’re excited to continue our work assisting and equipping schools to help keep children and their families healthy. The Back to School Toolkit builds on our two years of experience and brings our best resources yet to school leaders statewide.
Check out our Back to School 2015 Toolkit.
Originally Posted in Say Ahhh! A Children’s Health Policy Blog
By Sonya Schwartz
Now Playing: Coverage for more than 400,000 children and youth
Coming Soon: Coverage for more than 800,000 additional immigrant children, youth and parents
This week, Georgetown University’s Center for Children and Families and The Children’s Partnership released a new paper outlining how to get ready for big coverage opportunities in California. It highlights opportunities that will provide coverage to more than a million people in California’s immigrant families when immigration relief takes affect.
But as spelled out in the paper, Immigration Relief for Parents and Youth = Whole Family Health Coverage in California, while we wait for some of the immigration relief-related coverage options in California to become available, there is a lot that advocates and community organizations in California can do right now to cover eligible children and youth in immigrant families. Here is the run down of coverage opportunities “now playing” in California and also “coming soon” that could get many more children, youth and parents in immigrant families covered.
Now Playing: More than 400,000 children in immigrant families are already eligible for full scope or state-funded Medi-Cal but are not yet enrolled. It is not too soon to roll up our sleeves and get to work on covering them. Here’s the breakdown:
- More than 200,000 youth who qualify for the 2012 DACA program are estimated eligible for Medi-Cal but not yet enrolled. The initial DACA program announced in 2012 is for youth who came to the US before their 16th birthday; have continuously lived in the US since January 15, 2008; are at least 15 years old; are currently enrolled in school or qualifying adult education; or have graduated or obtained a certificate of completion of high school. Our estimates show that of the 343,000 youth qualified for the 2012 DACA program in California, 60 percent or 206,000 are uninsured and eligible for state-funded Medi-Cal. Not all of these 343,000 youth have applied for or been granted DACA status, but if they do receive DACA status and meet the income requirements, they are eligible for a state-funded version of Medi-Cal.
- More than 200,000 citizen or lawfully residing children in immigrant families are eligible for Medi-Cal but not yet enrolled. Our estimates show that 1.6 million children are living with immigrant parents who will be eligible for the new DAPA program in California. DAPA was announced on November 20, 2014, and, when implemented, will allow undocumented immigrant parents who have U.S. citizen or lawful permanent resident children, to apply for work authorization and protection from deportation, if the parent has been in the U.S. since January 1, 2010. Of those 1.6 million California children in DAPA families, 14 percent or 223,000 children are currently eligible for full scope Medi-Cal but remain uninsured. Reaching and enrolling these 223,000 children living in DAPA families would make a huge dent in the number of California’s uninsured children. This map shows that most of these DAPA families live in Southern California with the greatest concentration in Los Angeles County, followed by Orange County, San Diego County, Riverside County, and San Bernardino County.
Coming Soon: There are also opportunities to provide health coverage to more than 800,000 additional immigrant children, youth, and parents and the time to prepare is now. California just passed a law that will provide coverage to all children regardless of immigration status. And, when Deferred Action for Parents of Americans and Lawful Permanent Residents (DAPA) the 2014 expanded Deferred Action for Childhood Arrivals (DACA) program take effect, hundreds of thousands of children, youth, and parents will be eligible for state-funded Medi-Cal. People granted DAPA or DACA statuses are not eligible for federal matching funds for Medicaid or CHIP or for federal premium tax credits in the health insurance marketplace. However, California provides state-funded Medi-Cal coverage for persons residing under color of law (or PRUCOLs), and DACA grantees.
- 170,000 children in California will be eligible for state-funded Medi-Cal for children regardless of immigration status. California recently passed a budget bill (SB 75) that includes health coverage for all children up to 266 percent of the federal poverty level, regardless of immigration status. Children will enroll in a state-funded version of Medi-Cal and coverage will begin no sooner than May 2016. The expansion is estimated to cover 170,000 children.
- More than 600,000 parents in California will qualify for DAPA and likely to be eligible for state-funded Medi-Cal if granted DAPA status. More than 1 million parents in California are estimated to qualify for DAPA and 56 percent are low income by Medi-Cal standards and lack health insurance.
- More than 50,000 youth in California will qualify for the 2014 expanded DACA program and are likely to be eligible for state-funded Medi-Cal if granted DACA status. The expanded DACA program, announced on November 20, 2014, but on hold because of litigation, is also for youth who came to the US before their 16th birthday but who have continuously lived in the US since January 1, 2010 and meet other requirements. Estimates show that of 92,000 youth qualified for expanded DACA, 60 percent or 55,200 are uninsured and likely eligible for state-funded Medi-Cal.
If you are a children’s or immigration advocate or social service provider in California, our paper also provides specific suggestions about what you or your organization can do to help get children, youth, and parents in immigrant families covered. If advocates, service providers, and others working on health care, immigration, and child and family well-being work together to educate and enroll children and families in health insurance, it could lead to a significant reduction in California’s uninsured rate.
State-funded Medicaid coverage for DAPA and DACA grantees and the new coverage opportunity for children regardless of immigration status is unique to California and a few other states. But, all states cover citizen children in immigrant families. And, the majority of other states (twenty-eight) provide coverage to lawfully residing children in immigrant families. Although, there is always more work to be done get these eligible children enrolled in health coverage.
Continue reading on the Georgetown Center for Children and Families website.
For most of his childhood, Ethan and his mother often had to drive six hours from their home in Redding, California, to Los Angeles to meet with a psychiatrist for his autism treatment. Today, Ethan, now 19 years old, drives just 10 minutes to a clinic in Redding where he meets with the very same psychiatrist via a live video conferencing system.
Telehealth, using technology to provide health care and support services at a distance, has the potential to improve care for the 1.4 million children in California who, like Ethan, have special health care needs. These children often require multiple specialists, coordinated health care, and related services on an ongoing basis. In both rural and urban areas of the state, Children with Special Health Care Needs (CSHCN) often find their health care needs unmet for a variety of reasons, such as provider shortages, lack of access to specialists, lack of affordable transportation, and a number of other barriers. But with the increased use of video conferencing, remote patient monitoring through smartphones, and other technology applications, we can break down those barriers and make it possible for more children to get care they may otherwise go without, right in their own communities.
Recognizing the potential of telehealth, The Children’s Partnership, the UC Davis Children’s Hospital, and the Center for Connected Health Policy, with support from the Lucile Packard Foundation for Children’s Health, set out to understand how telehealth is currently being used to meet the needs of California’s CSHCN and identify where policy constraints to wider adoption exist. After conducting a literature review, online surveys, and interviews with key stakeholders, including providers and California Children Services (CCS) administrators, we were able to uncover both the best practices of how telehealth is implemented and the difficulties in bringing it to scale.
The majority of providers surveyed, namely pediatric physicians, thought telehealth has potential to bridge gaps in care for CSHCN, but over 50 percent felt that issues of time, reimbursement, and equipment limited its use. Of the 39 CCS program administrator respondents, 32 out of 39 would be interested in state-sponsored training to learn more about telehealth.
It was clear from our interviews and surveys that many are eager for an expansion of telehealth that could help families get their children the care they need in a timely manner and at an affordable cost, regardless of where they live. CSS, health care providers, family advocates, children’s advocates, philanthropists, and other stakeholders all have a role to play to make telehealth for CSHCN a reliable option throughout California. Through expanded outreach to families and providers, and increased incentives for participation, we hope to have more success stories like Ethan’s, so instead of driving hours to multiple doctors’ appointments, children can spend their time reaching their potential.
Read “Realizing the Promise of Telehealth for Children with Special Health Care Needs.”
Today marks 50 years since Medicaid was signed into law and it is truly a day to celebrate. The program has had a long, successful history of bringing health care to children and families most in need. A combined federal-state effort to finance health programs and ensure timely care, Medicaid provides coverage for nearly 33 million children, or 37 percent of all children living in the United States. All of these children are able to get regular preventive care, from well-child visits and immunizations to dental, hearing, and vision care. And Medicaid provides services for children with special health care needs as well.
Now that longitudinal data is available, we can squarely say that the benefits of providing health care go far beyond the doctor’s office. In honor of the occasion, our partners at The Georgetown Center for Children and Families released a report detailing the growing body of research that shows the long-term benefits Medicaid has provided to children and the nation. Children with access to Medicaid are proven to have better health as adults, with one study showing a 26 percentage point decline in the incidence of high blood pressure in adulthood. Enrollment in the program is also associated with greater academic achievement and higher likelihood of graduating from high school and college. And recent studies suggest that giving low-income kids access to health coverage boosts their future earnings for decades, therefore increasing their future income tax contributions and helping generate an even bigger return on investment.
California is leading the way in giving families peace of mind, knowing that their children have health coverage that allows them to be healthy and productive. Thanks to recent action, starting no sooner than May 2016, California will cover the last remaining group of uninsured children—those who are undocumented. This will ensure more kids in the state than ever before can get a fair shot in life and will help reduce California’s still-unacceptable 7.4 percent children’s uninsurance rate in the state.
In California, and across the nation, we need to continue to both protect and expand Medicaid. The benefits to children’s health, education, and long-term prosperity could not be clearer. On the fiftieth anniversary, let’s commit to keeping Medicaid strong for future generations of children.
Good oral health is critical to children’s ability to grow up healthy and succeed in school and life. Yet, dental disease remains the number one chronic health problem among children. And the numbers are particularly worrisome for our youngest.
Despite the availability of dental care through Medi-Cal, California’s youngest children do not receive the dental care they need. Nearly 1.7 million children aged 0–5 are enrolled in the program and, in 2013, 63 percent did not have a dental visit in the past year. This is unacceptable when we know that early preventive dental care results in better oral health, overall health, and well-being over one’s lifespan. By the time children reach the third grade, 71% have experienced tooth decay.
While there are many roots to this problem, a leading issue is the lack of providers. Many providers are not willing to provide dental care to young children enrolled in Medi-Cal due to low-reimbursement rates. Even those open to serving children often deny services for three-year-old children. And when many younger children do get care, they are not getting appropriate care for their age. Pediatric dentistry encompasses disciplines, techniques, and skills required to meet the unique needs of young children based on their developmental level, including behavior guidance and sedation.
The Children’s Partnership is working with the First 5 Association to ensure full access to dental health care for California’s youngest children. Here are the 123’s for the Legislature and Administration to fix this dental care crisis our 0–5 year olds are facing:
- Invest in the Virtual Dental Home (VDH) to bring dental care to where children are—start by enacting AB 648.
- Provide financial incentives to providers that expand access to essential dental services for the youngest children enrolled in Medi-Cal.
- Ensure the Department of Health Care Services implements the recommendations to increase utilization of dental services identified in the recent state audit of Medi-Cal’s dental program.
Download the fact sheet “Addressing the Oral Health Needs of California’s Youngest Children”.
Download our new infographic. (PNG | PDF)
In 1997, The Children’s Partnership joined with a small group of children’s advocates and supporters and set an audacious goal—securing health coverage for every child in California. With a name that was aspirational, accountable, and determined, we called our effort the “100% Campaign.”
When our journey began, California had nine million children, and 1.74 million of them (nearly one in five) had no health insurance. The reasons varied from lack of affordable coverage options, to a 28-page application form, to policies that precluded eligibility for most immigrant children.
During this time, the Clinton Administration’s effort to enact health care for all Americans was blocked, and the bipartisan Children’s Health Insurance Program (CHIP) emerged to address the needs of children whose families make too much money to be covered by Medicaid, but cannot afford private insurance. Meanwhile, California was battling a voter-passed initiative (Proposition 187) in the courts that would have denied most public benefits to immigrants without documentation. At this juncture, our campaign knew there would be an uphill climb to this goal.
The 18-year trek included numerous efforts and hard-won, step-by-step progress—a testament to the persistent, at times creative and at times heroic efforts of policymakers and their staff, foundations who stayed the course, health providers, community organizers, and consumer advocates. Beginning in 2001 with a local pilot in Santa Clara County that demonstrated the health and cost benefits of covering all kids, local Children’s Health Initiatives were expanded over time to become available to children in 30 of California’s 58 counties at their peak. A dedicated group of California leaders tried most every tack possible, including a state legislative and budget effort, a tobacco tax measure on the 2006 ballot, and an attempt by Governor Schwarzenegger to enact state health reform. But budget setbacks, tobacco industry opponents, and legislative opponents frustrated the progress.
Amidst these attempts that came close to covering all kids but failed, impressive progress was made over the years. The Healthy Families Program—California’s CHIP—grew to provide subsidized coverage to hundreds of thousands of children in working families; the 28-page application form was replaced by a far shorter one; and Express Lane Eligibility made it easier to enroll large numbers of uninsured children already certified for other income-tested programs like the National School Lunch Program in health coverage programs. The passage of the landmark Affordable Care Act in 2010 opened up coverage options to many more families, but still the job was not complete.
Even with setbacks, we were not defeated, our resolve strengthened with the knowledge that the public was in favor of coverage for all kids, including undocumented immigrants.In 2005, four out of five voters (78 percent) supported a statewide plan to “ensure that every child in California has health insurance,” with more than half (55 percent) saying they “strongly support” it. In 2014, a majority supported expanding existing health care programs to cover all low-income Californians, regardless of immigration status.
After nearly two decades, policymakers’ actions caught up with public support. Last week, a historic budget was signed by Governor Jerry Brown extending health benefits to undocumented children. Now, we can finally say the original goal of securing coverage for 100 percent of California’s children is a practical reality.
Any good advocate will point out that the job isn’t finished as we work to implement these changes and actually enroll children, and to be sure that securing health coverage translates into meaningful access to health care and improved health for children. In addition, it is time for policymakers to step up and support offering affordable coverage for family members as well as children.
But, it is just as important to herald this moment and acknowledge the work of our state leaders and countless others to achieve a goal so important and so right as making sure that every child in the Golden State has a chance to grow up healthy. It is a 100 percent great moment for California and our kids.
Originally Published in First Focus: Voices for Kids.
Despite the successful implementation of the Affordable Care Act two years ago, over one million individuals remain uninsured in California simply because of their immigration status. But that number could change shortly thanks to unprecedented momentum in favor of health for all in the state. Two weeks ago, the California State Senate made history with a 28-11 vote in favor of a bill that would be the first step to ensure health coverage options to undocumented immigrant residents. With ayes from both sides of the aisle, the bill now moves on to the Assembly. And last week, the California legislative budget conference committee voted to provide $40 million to extend Medi-Cal to undocumented children. Now, the question is whether the legislative leadership will hold firm and send the bill and the budget with this funding to the Governor—and whether the Governor will sign them.
SB 4, authored by California Senator Ricardo Lara, would allow undocumented immigrants to purchase health insurance through the state’s health care marketplace (with a section 1332 waiver from the federal government) as well as provide coverage for low-income children through Medi-Cal, California’s Medicaid program. Low-income adults can also qualify for Medi-Cal, but enrollment is capped based on available funds. An estimated 170,000 undocumented California children could receive comprehensive care as a result.
By offering affordable insurance options to immigrant family members, the whole family is more likely to enroll, including their citizen and lawfully present children who already qualify but are not yet enrolled in coverage. One in six kids in California has an undocumented parent locked out of health coverage, and the majority of these children are citizens. When parents get health coverage, their children are much more likely to be enrolled and to get preventive care.
More and more, leaders are recognizing that investing in the health of hardworking immigrant parents and their children has substantial long-term impacts that benefit all Californians. States already provide emergency care coverage for undocumented immigrant residents, even though preventive care and early treatment are far superior and much more cost effective. A growing body of research shows that if every single parent and child had preventive and ongoing care, we could reduce overall health care costs, avoid preventable emergency room visits, and foster more productive communities. Providing full-scope Medi-Cal coverage would cost less than Medi-Cal emergency services coverage the state is currently providing for undocumented immigrant children.
A study of local programs that extended health care to low-income children estimated that 6,324 childhood hospitalizations were prevented over a five-year period, resulting in approximately $6.7 million in savings to the health care system. Moreover, children need regular checkups to assess healthy childhood development and identify and treat problems early.
When children have health coverage, they are considerably more likely to graduate from high school and complete college. Children newly enrolled in health coverage pay closer attention in class, resulting in a 63 percent improvement in school performance. Expanding health care to undocumented immigrants truly is the remaining piece in ensuring all of our kids are healthy and ready to learn.
The recent Senate vote reflects the opinion of the vast majority of Californians across the political, geographic, and demographic spectrum—undocumented immigrant children should have access to affordable health coverage options. A majority of Californianssupport affordable health options for all low-income undocumented immigrant residents. The broad and diverse coalition of Californians—from business leaders, churches, health care providers, workers, and families across the State—will be watching and urging our policy makers to support options for the remaining uninsured. If SB 4 is enacted into law, California will continue to demonstrate its leadership in laying the foundation needed to extend health care coverage to all. We hope California finishes the job and brings health coverage to all Californians and that other states shortly follow suit. Extending coverage to all children and families is not only cost effective—it’s the right thing to do.
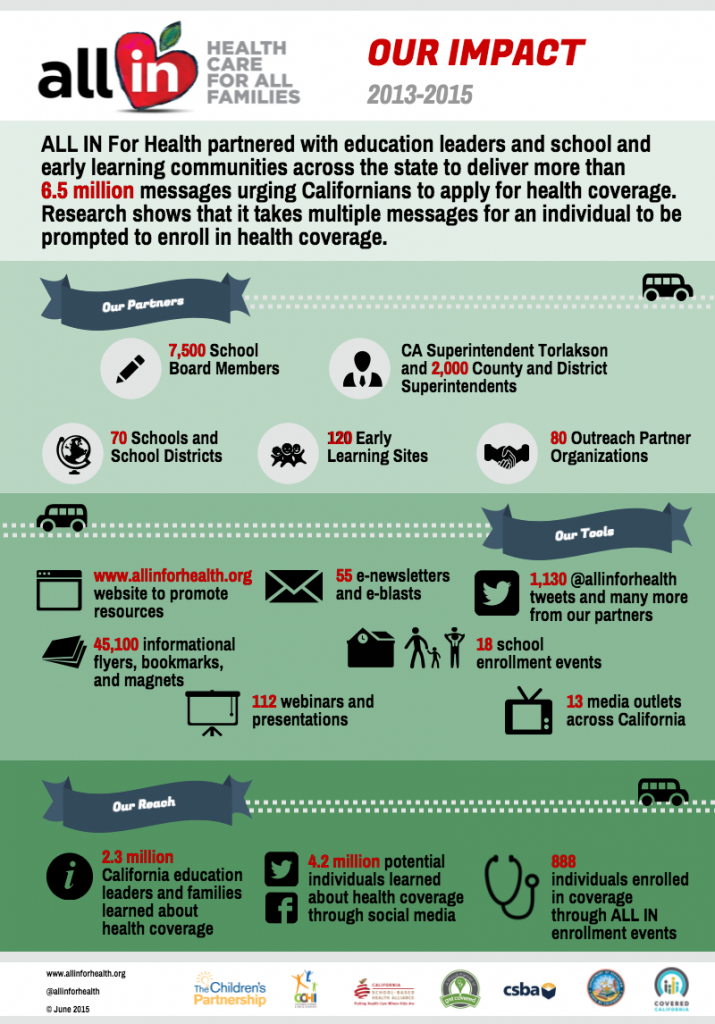
Lessons learned from two years of the ALL IN For Health Campaign
When the education and children’s health advocacy leaders in California came together two years ago to partner for student and family health, no one knew what the outcome would be. As California was preparing to roll out new health coverage options for families and individuals as part of health care reform in summer 2013, California State Superintendent of Public Instruction Tom Torlakson partnered with The Children’s Partnership. Together, we called on the state’s education leaders to work with child health advocates to help families connect to new health coverage options. The message was that no one knows better than teachers, school personnel, and other education leaders that healthy children make better learners.
As a result of this call to action, The Children’s Partnership launched the ALL IN For Health Campaign with a simple mission: equip schools, early learning centers, and after-school programs with the tools they need to help more kids and families enroll in health coverage. At the time, California was gearing up to launch its first open enrollment period through Covered California, the state’s Health Benefit Exchange, and provide more Californians with coverage through expanded Medi-Cal, California’s Medicaid program. With new affordable health care options coming to families across the state, ALL IN For Health identified schools, early learning centers, and after-school sites statewide as places where thousands of families could learn about their new options and find out how to enroll in a plan that meets their needs.
This model has proven to be highly successful; over the last two years, with our partners in the education community, ALL IN For Health has delivered more than 6.5 million messages across the state informing families about health coverage options and how to enroll, and encouraging them to take action to get covered. Research has shown that consumers need to be prompted multiple times before they enroll in coverage, making ALL IN’s voice an important one in the push to get more Californians covered.
In the past couple of years, we’ve learned some valuable lessons about what works in partnering with the school community to reach families and students with important health information. For example, we learned that partnering with well-respected leaders in the education community and offering them an easy-to-implement game plan with off-the-shelf materials is vital for getting buy-in and making sure these leaders can easily engage in outreach activities. We also learned that speaking the schools’ language and tying activities to the school calendar really works in getting more families enrolled in health coverage.
Check out our Summary Report for more details on what we’ve learned and ideas for how you can bring a campaign like ALL IN to your community. Not convinced yet? The numbers in our infographic speak for themselves.