The social and emotional well-being of California’s students has come under increasing strain in recent years. From COVID-related isolation to rising rates of anxiety and trauma exposure, students are navigating complex challenges, often without adequate mental health support.
In response, peer support and peer-to-peer mentoring have emerged as promising, evidence-based approaches for enhancing student engagement, destigmatizing mental health services and fostering a sense of community.
To better understand and expand the potential of these approaches, BBDKSM, in partnership with The Children’s Partnership, is conducting an expansive evaluation of TCP’s Peer-to-Peer Youth Mental Health High School Pilot Demonstration across eight diverse high school sites in California: Sierra Continuation, DaVinci RISE, Mission Hills, Serrano, Oakland Technical, Nevada Union, El Cerrito and Antioch. This report shares key themes and findings from Year 1 of the pilot demonstration, and is one of several to be released during the evaluation of the pilot ahead of the final evaluation report.

The Children’s Partnership’s policy brief, “Uplifting the Power of Culture: Protective Factors for the Health of California’s Children,” highlights how culturally grounded protective factors in early childhood can create equitable pathways to health and success for BIPOC children. Grounded in research and real-world examples, the brief:
- Highlights key protective factors for children of color, including multilingualism, connection to culture, peer and community connectedness, familismo, and cultural-based healing
- Explores how California’s early care and education programs can integrate these protective factors to strengthen child, family and community well-being
- Provides actionable recommendations for policymakers and advocates to build equitable systems of care that reflect the unique strengths of BIPOC communities
- Underscores the critical role of culturally responsive early care programs in promoting resilience and mitigating the impacts of systemic inequities
By centering protective factors in early childhood programs, California can help ensure all children—especially those from marginalized communities—have the support they need to thrive.
As policymakers and advocates work to create inclusive and supportive systems, we invite you to explore this resource and share it with your networks to amplify the conversation around protective factors and their vital role in equitable early care for children.

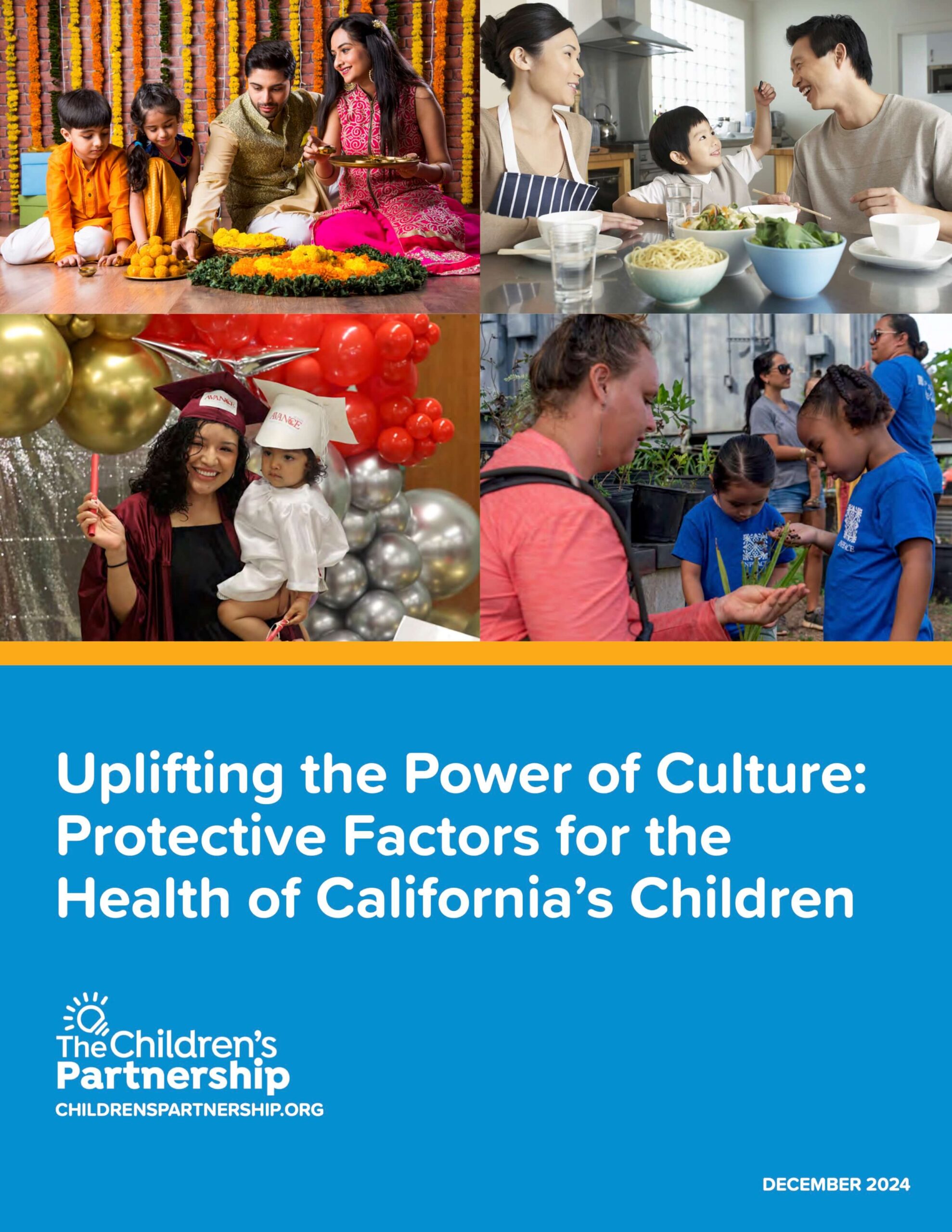
The Children’s Partnership has created a fact sheet to help youth 12 and older better understand their new right, established through AB 665, which allows them to consent to outpatient mental health services and bill their existing Medi-Cal insurance.
AB 665 was a bill created by youth and for youth to bridge a gap between Medi-Cal and privately insured youth in accessing minor consent mental health services. Minors’ right to consent to outpatient mental health care was established through a prior bill, SB 543. However, SB 543 created a higher standard of need for youth on Medi-Cal in order for the provider to bill Medi-Cal for mental health care services. This fundamentally unfair double standard meant that low-income youth were required to wait until they were experiencing a mental health crisis before they could receive confidential, Medi-Cal-covered care.
AB 665 changed that. Now minors have the ability to consent to and use their existing Medi-Cal insurance to cover outpatient mental health services without needing their parents’ authorization, just like privately insured youth. This will greatly benefit youth across California by increasing access to timely services for historically marginalized youth, including BIPOC and LGBTQ youth.
This fact sheet offers:
- Guidance on accessing and navigating mental health services for youth on Medi-Cal
- A simple and easy-to-read explanation of AB 665: Mental Health Consent Parity for Medi-Cal Recipients
- Medi-Cal assistance
- Information on what youth can do if they are denied services
AB 665 was co-sponsored by The Children’s Partnership, California Alliance of Child and Family Services, California Children’s Trust, Cal Voices, GENup, and the National Center for Youth Law.

Making Medi-Cal Work for Families: Keeping Children Covered
Stable health insurance coverage is necessary for the continuity of health care. With the majority of California children relying on Medi-Cal for their health coverage, continuous Medi-Cal coverage plays a critical role in children’s healthy early childhood development. Medi-Cal is also pivotal to child health equity as three-fourths of Medi-Cal children are children of color.
But Medi-Cal currently requires families to renew their eligibility every year. While a lot has been done to streamline this renewal process, too often children and families lose their Medi-Cal coverage – not because they no longer qualify but due to administrative barriers and glitches, such as not receiving renewal packets in the mail or long call wait times.
Data Brief: How Continuous Medicaid Coverage Protected California Children
A TCP brief, “Learning From the Pandemic: How Medi-Cal Continuous Coverage Protects California Kids,” demonstrates the success of the federal continuous coverage provision in keeping millions of Californians enrolled in Medi-Cal coverage during the COVID-19 pandemic and what is at stake for children and families when the protection ended in April 2023.
This brief also highlights recommendations to help the state minimize disruptions to children’s coverage, such as moving forward with the implementation of multi-year continuous Medi-Cal coverage for children ages 0-5.
Since the unwinding began, over 300,000 California kids have lost Medi-Cal.
Focus Groups: How Gaps in Coverage Impact Children and their Families
As we witness California children losing coverage as Medi-Cal annual redeterminations start up again, TCP wanted to raise parent voices to speak to what are the very real impacts of gaps in health coverage on children and their families. We commissioned Lake Research Partners to conduct 10 focus groups with over 80 parents/guardians of children of color to share their experience with what it means to be without insurance coverage – even for a short period.
Listening to families themselves advances health equity by identifying how the process can work for them, not just for the system.
Learn more in our summary slide deck.
Focus Groups: Families Share What Works and How to Fix What Does Not
As all Medi-Cal enrollees go through annual eligibility renewals for the first time in three years, the aggregate disenrollment data shows more than 306,000 children have lost coverage (June 2023-February 2024). We wanted to hear directly from families about their renewal experience during the unwinding period.
The Children’s Partnership commissioned Lake Research Partners to conduct ten focus groups of families of color and two groups with Medi-Cal enrollment assisters to hear about their renewal experiences – what worked and what needs to be fixed. These families and assisters provided pragmatic recommendations for how to make the system work better. A summary of this wealth of information can be found below.
Study: Research Reveals Long Medi-Cal Call Wait Times, Undermining Access to Coverage
The Children’s Partnership commissioned WestGroup Research to survey Medi-Cal call wait times because we heard from enrollees and community-based organizations that families across the state were not able to get through to Medi-Cal – often waiting up to two hours on the phone.
Keeping coverage requires a program that works for enrollees. This seminal research found long call wait times and high dropped-call rates in several counties, as well as examples of stellar customer service that could serve as model strategies for how to make Medi-Cal work better for families.
Advocacy
Multi-Year Continuous Coverage Budget Proposal
California has adopted a multi-year continuous Medi-Cal enrollment protection for young children. This will enable children under the age of five to keep coverage without annual renewal requirements that can cause harmful health care gaps. To meet the January 2026 start date for this policy, we urge the Governor to direct the Department of Health Care Services to submit a request for federal approval now.
Support
A coalition of organizations came together to advocate for implementing continuous Medi-Cal coverage for young children:
The Children’s Partnership
American Academy of Pediatrics-CA
Children Now
First 5 Association of California
March of Dimes
Maternal Child Health Access
National Health Law Program
Western Center on Law and Poverty
We are joined by over 60 other organizations across the state supporting funding this preservation of children’s coverage. Here is a collective support letter.
Stable health coverage is a core racial equity strategy. The Whole Child Equity Partnership (WCEP)–a coalition dedicated to a society rooted in racial and economic justice–is working to make California the best state to have, raise, and be a child. One of their policy priorities is implementing multi-year continuous Med-Cal coverage. Here is their support letter.

Medi-Cal Call Wait Times Survey Report
Keeping Medi-Cal coverage is not easy. Many enrollees lose their coverage not because they no longer qualify but due to administrative barriers, such as not being able to connect with a Medi-Cal worker over the phone to renew their coverage.
The Children’s Partnership commissioned WestGroup Research to survey Medi-Cal call wait times because we heard from enrollees and community-based organizations that families across the state were not able to get through to Medi-Cal – often waiting up to two hours on the phone.
Keeping coverage requires a program that works for enrollees. This seminal research found long call wait times and high dropped-call rates in several counties, as well as examples of stellar customer service that could serve as model strategies for how to make Medi-Cal work better for families.

Our latest brief in partnership with the First 5 Center for Children’s Policy provides an update on Medi-Cal’s community health worker (CHW) benefit implementation, as well as uplifts programs and models across California that are utilizing CHWs, promotores and representatives to benefit children and families across the state. We also share policy recommendations, including how we can continue to take successful models to scale, in line with the CHW/P/R Coalition.

9-8-8 Fact Sheet
We are excited to introduce the 988 Suicide & Crisis Lifeline Fact Sheet! The 988 Lifeline provides compassionate, accessible care and support for people experiencing mental health-related distress.
The fact sheet is a valuable resource for community-based organizations and schools:
- Outlining the importance of shifting from a discipline response to a care-and-compassion response for students struggling with stress, depression or suicidal behaviors;
- Providing information on how 988 can be utilized by anyone experiencing mental health challenges, as well as by third parties concerned about a friend, student or loved one;
- Offering practical guidance on how schools can implement 988 as part of their suicide prevention and mental health policies and protocols.
Use this fact sheet to raise awareness about the 988 Lifeline! By sharing this resource widely, we can help ensure that individuals in need have access to the support and care they deserve.
Thank you to our partners in this effort: California Black Women’s Health Project, Didi Hirsch, and The California Alliance of Child and Family Services.

Feedback Loop
FEEDBACK LOOP
MEDI-CAL UNWINDING & RENEWALS RESTART
Monthly virtual opportunities to share your experiences with Medi-Cal renewals. Attendees can ask questions, get updates and share feedback.
Register here: https://bit.ly/RenewalFeedbackLoop
Do you work with California communities on Medi-Cal? Do you assist individuals and families with Medi-Cal enrollment and renewals? We are here for you and want to hear from you!
As Medi-Cal renewals resume, The Children’s Partnership (TCP) & the National Health Law Program (NHeLP) are hosting a feedback loop to identify and help address issues and concerns with the renewal process.
If you are a community-based organization, health care navigator, enrollment assister, community health worker/promotora, provider, or other advocate on the ground, please join us. Our virtual meetings will take place every month following December, starting at 12 p.m. PST:
- December 13, 2023
- January 24, 2024
- February 28, 2024
- March 27, 2024
- April 24, 2024
- May 22, 2024
- June 26, 2024
- July 24, 2024
- August 28, 2024
Interpretation services will be provided upon request.
Please register here: https://bit.ly/RenewalFeedbackLoop
Questions?
Contact:
Kristen Golden Testa – ktesta@childrenspartnership.org
Skyler Rosellini – rosellini@healthlaw.org

NEW REPORT:
Telehealth and Children of Color with Special Healthcare Needs: Lessons from the Pandemic
Children of color and children in immigrant families make up over a majority of children with special health care needs (CSHCNs): 71% of the state’s CHSCNs also identify as Latinx, Black, Indigenous, Asian American, Pacific Islander, or Mixed Race, making up nearly 1 million children. Yet despite the size of their population, there is a lack of statewide research or policy focus on the needs of this population of children. TCP’s report, Telehealth and Children of Color with Special Health Care Needs: Lessons from the Pandemic, utilizes a community-centered approach to create a policy agenda that centers the lived experiences of families and children of color with special healthcare needs in California.
The learnings from the report provide unique insights into the experiences and challenges they and their families faced during pandemic shutdowns, including in the use of telehealth to access care. The report also sets forth actionable policy recommendations rooted in the experiences and recommendations of families of color with children who have special health care needs.

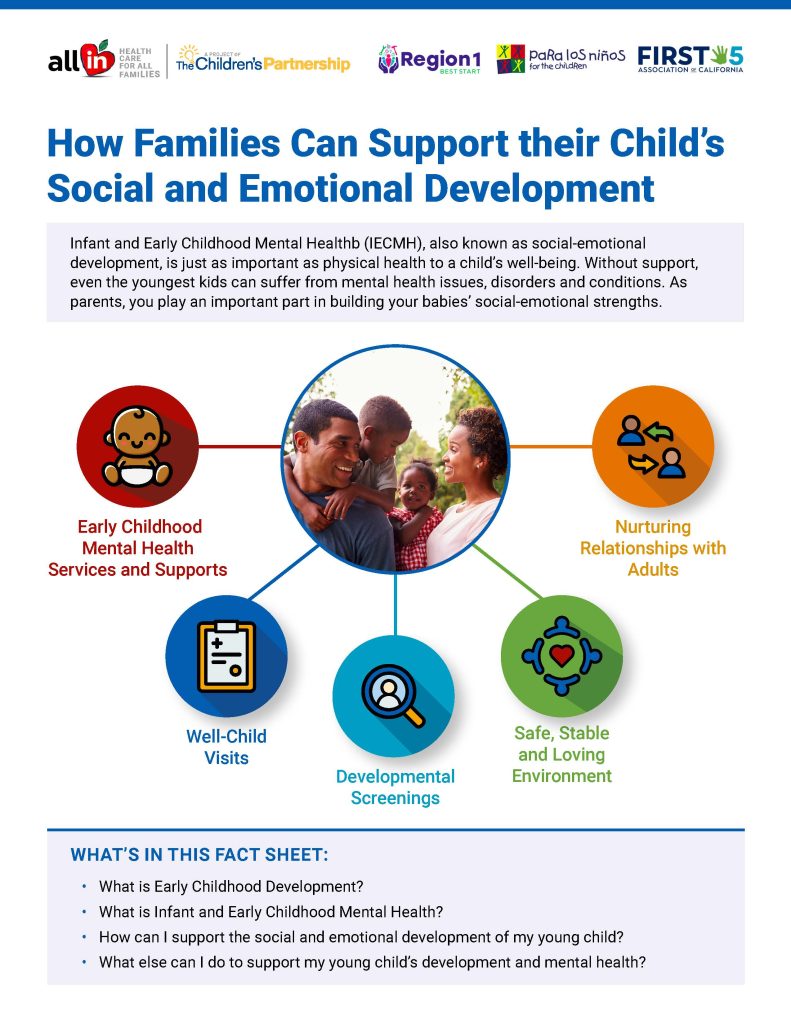
How Families Can Support their Child’s Social and Emotional Development
Infant and Early Childhood Mental Healthb (IECMH), also known as social-emotional development, is just as important as physical health to a child’s well-being. Without support, even the youngest kids can suffer from mental health issues, disorders and conditions. Parents play an important part in building your babies’ social-emotional strengths.
In partnership with First 5 Association of California, Para Los Niños and Best Start Region 1, we are releasing a new community resource: “How Families Can Support Their Child’s Social and Emotional Development.” This community resource is intended to help parents, caregivers and family members of infants and toddlers support their child’s early mental health and social-emotional development.