For decades, community organizations, policymakers, and advocates have worked together to make sure every member of the family could experience the benefits and security that health coverage provides. Families have bravely made their voices heard to make sure their kids could lead healthy and happy lives and the state of California is listening. Last year, the first victory in the journey toward health for all was achieved—all children, regardless of immigration status, will soon get free or low-cost health coverage through Medi-Cal. If a child under the age of 19 meets income guidelines, he or she will qualify for Medi-Cal. As we celebrate this milestone, we must continue our work to educate families, build awareness, and make sure every family takes advantage of this important opportunity.
Although the expansion of benefits to all children is expected later this year, families can act now to make sure that their kids get the comprehensive health coverage they need as soon as possible! Families can begin enrolling their children in restricted Medi-Cal (also known as emergency Medi-Cal) TODAY. Then, once the expansion is in place, those children enrolled in restricted Medi-Cal will be automatically enrolled into full-scope Medi-Cal. Families can apply without fear and know that their immigration status information is kept private. To enroll, immigrant families should visit www.localclinic.netto identify a local clinic to apply at or visit their local county human services office.
The expansion of Medi-Cal will help thousands of California children, but many families have questions and concerns about applying. The ALL IN For Health Campaign—the TCP-led effort to equip the education community with tools to help families connect to health coverage and care—has created a new flyer for schools to distribute to families. The flyer includes the most important facts about the expansion of Medi-Cal to undocumented children and how to get enrolled today. With our school and early learning partners, we can reach many of California’s more than 9 million children, including this newly eligible population, encourage families to enroll in restricted Medi-Cal now, and connect them to enrollment assistance. We also plan to continue learning about how we can better reach families with this information. We want to do all we can to work with trusted community centers, such as churches, clinics, small businesses, and more to help get the word out that it’s safe to apply.
Getting more kids enrolled in health coverage is key to children getting the care they need to grow up healthy. When children have health coverage, they can get preventive care that catches potential health issues before they become a problem. It also enables families to build a relationship with a doctor, dental provider, or other health care provider so that they have someone to call on when health issues do come up. Finally, children with health coverage are much less likely to miss school and are better prepared to learn and succeed in the classroom!
We hope you will join us in making sure all families have this important information and take the next step to enroll their kids in coverage. And, together, we will work toward a statewide solution so that all Californians, both children and adults, have access to quality, affordable coverage. Help spread the word by sharing “The ABCs of Health Coverage for ALL Kids” with your community.
Learn more about the Health for All Kids Medi-Cal Expansion.
Learn more about #Health4All and expanding coverage to all Californians.
As the new President of a dynamic and innovative children’s advocacy organization, I am constantly learning—from community members, partners in the field, policymakers, my staff, and many others. At TCP, it is our organization-wide commitment to learning that informs our work to better meet our primary goals of ensuring all children have access to quality, affordable health care and reap the benefits of digital opportunities. To learn more about our work, I invite you to take a look at our recently released California and Federal Policy Agendas, where we as an organization have the chance to make good on our mission to improve the health and well-being of children in the Golden State and across the nation. These agendas reflect how what we are learning influences our work as we continue to evolve with the changing political and social landscape for children.
In 2016, we will build upon TCP’s two-plus decades of work to continue securing key advances for children across the nation. I’m excited to work with our partners to ensure that all children have quality health coverage that meets their needs. This includes continued work in California to make certain that children’s voices are heard as the implementation of the Affordable Care Act moves forward, as well as in the implementation of the recent extension of Medi-Cal to all-low income children, regardless of immigration status, and in the work of refining processes to make obtaining coverage as seamless as possible for every family that qualifies. Nationally, we will continue to advocate so that the crucial and bipartisan Children’s Health Insurance Program’s success in providing affordable, child-specific, and comprehensive coverage continues.
For this work and more, we recognize the importance of reaching families in their communities as key to a successful outreach effort to ensure newly eligible children and families enroll in health coverage and access preventive care. From community-based organizations to government agencies to private companies, we will continue to partner with diverse organizations to make sure families have the information they need to access health coverage and care. Our ALL IN For Health Campaign has already delivered 7.3 million messages to families encouraging them to enroll in affordable health coverage, thanks to the help of partners in the education community. In the coming year, we will deliver even more messages with the help of our partners.
We will also continue promoting the smart use of technology to improve the quality of care received by our most vulnerable children and to empower families to take control of their children’s health. And we will keep pushing to ensure that the 5.5 million California children enrolled in Medi-Cal receive the dental care they deserve—especially considering that dental care is the number one unmet chronic health care need for children.
When I took the helm of The Children’s Partnership late last year, I brought with me my personal and professional mission of ensuring families are healthy and able to pursue their dreams. I am excited to learn from families in California about how our work moving forward can better meet their needs. These policy agendas reflect what our team has heard and represent our next step toward making that mission a reality. We hope you will take the time to read them and learn a bit more about TCP and our work this upcoming year.
Read our California and Federal Policy Agendas for 2016.
Healthy students make good learners. That’s the logic behind The Children’s Partnership’s ALL IN For Health Campaign, an effort to equip educators with the tools they need to connect children and families to health coverage and care. We’ve heard the impact of health on kids’ ability to learn from on-the-ground stories, including teachers who have seen students rack up absences and, as a result, fall behind in school. These are children who don’t get the health care they need or whose toothache or poor vision prevent them from concentrating in class. Many of these children don’t have health coverage and, thus, are not getting preventive or timely care when they have a health problem.
Health coverage and care are key elements to making sure that students are in class and ready to learn. Students with health coverage are more likely to graduate from high school, go on to college, and contribute more in tax revenue as adults. The understanding that health is a key component to school success is now fueling a new federal initiative. Late last week, the US Department of Education (ED) and the US Department of Health and Human Services (HHS) announced Healthy Students, Promising Futures. This campaign offers schools a number of high-impact opportunities to improve the health of their students, from connecting eligible students to health coverage opportunities to promoting healthy practices through physical and health education.
As a result of the Affordable Care Act, millions of children and adults now have health coverage. And now that students have that coverage, schools have the opportunity to move students up the wellness continuum, beyond the point of simply not being ill to being truly well. They can do this by connecting students to preventive care and educating them on healthy habits. ED and HHS recommend delivering health services to students directly in schools, providing support services and case management to at-risk students, and partnering with local hospitals and organizations. And, by promoting healthy habits such as eating well and engaging in physical activity, schools can encourage healthy habits that last a lifetime.
At The Children’s Partnership, we share the Administration’s commitment and have acted on it through our ALL IN For Health Campaign. To reach as many families as possible, we’ve enlisted the leadership of the California State Superintendent of Public Instruction, Tom Torlakson, and partners like California School Boards Association, California Parent Teacher Association, and California Head Start Association, among many others, to help connect schools and early learning sites across California to the information and materials they need to help families understand their coverage options and help them enroll. As a result, we’ve been able to deliver over 7.3 million messages informing families about their health coverage options and how to enroll and connect to care.
We applaud the Obama Administration for highlighting and supporting this high-yield connection between health and education and look forward to seeing what can happen when more schools and members of the health care community partner to help every student in the country thrive.
If you’re a school or early learning center in California, use our toolkit to help eligible students and family members enroll in affordable health coverage. And learn more aboutThe Children’s Partnership’s experience in conducting a statewide campaign that partners health advocates and the education community in order to benefit the children and families they both serve.
When I worked at the US Department of Health and Human Services, I was fortunate to travel coast to coast helping educate Latino families about how to enroll in quality, affordable health coverage through the Affordable Care Act. Mothers and tías, fathers and abuelitas would share their stories, their challenges, and their hopes about what the ACA could do for their families. I often talked about my baby sister and how, through the expansion of Medi-Cal, she was able to enroll in coverage and have one more tool to help make sure she can lead a healthy life. Our shared stories reflected the hope we all have for our loved ones—that they be able to lead healthy lives. And since the passage of the ACA, we have made real progress for the future of the Latino community and, in so doing, the state of California.
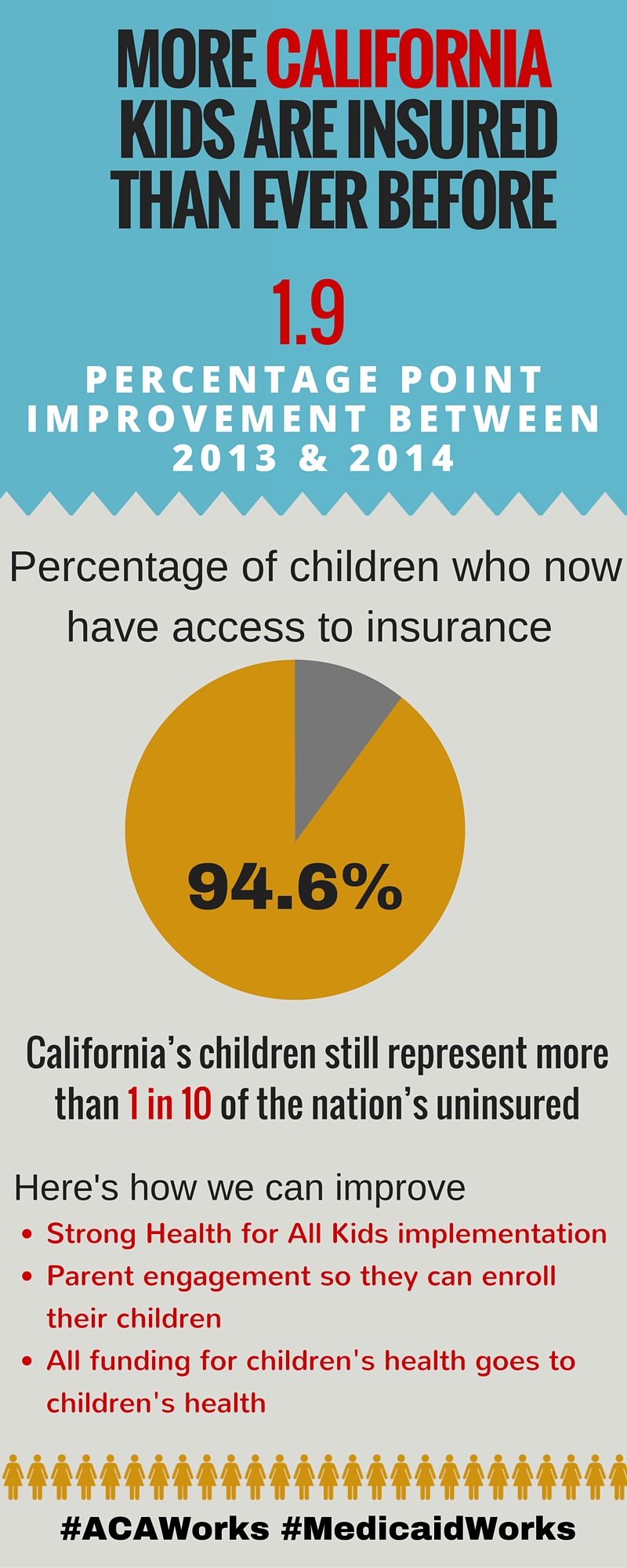
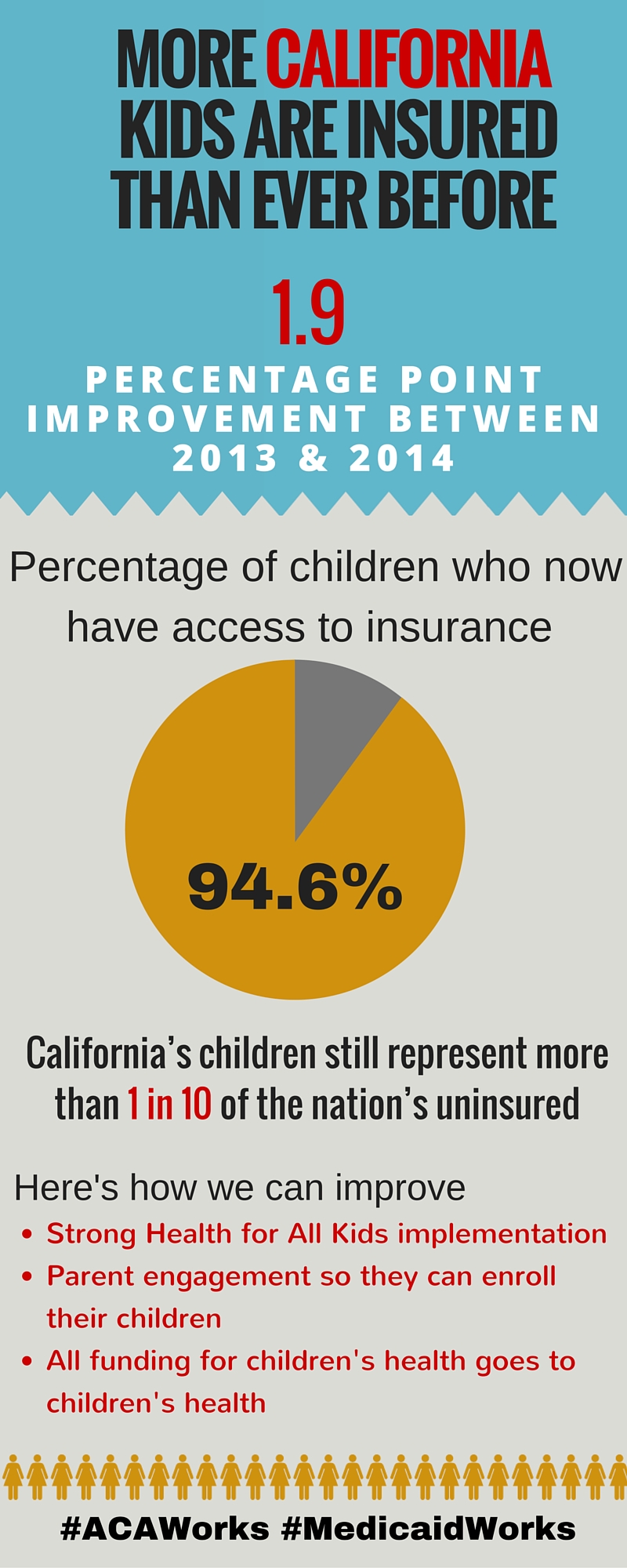
In California, Latino children make up half of all children under the age of 18. The future of California depends on our ability to ensure their health and well-being. A new report,Historic Gains in Health Coverage for Hispanic Children in the Affordable Care Act’s First Year, shows that the number of uninsured Latino children dropped dramatically in the first year that the ACA took effect, and California led the way, accounting for more than one-third of the national reduction. Released by the Georgetown Center for Children and Families, the National Council of La Raza, and the California Children’s Health Coverage Coalition, the report shows the uninsurance rate for California’s Latino children declined from 9.6 percent in 2013 to 6.8 percent in 2014, a rate significantly lower than the national average of 9.7 percent.
Through the collaborative work of community-based organizations, health centers, churches, promotoras, families, and many others, California made important strides in reaching Latino families and enrolling Latino children. Trusted organizations opened their doors and walked families through the enrollment process. Familiar sources of information shared important details like key dates and answered questions about ways to apply. California opened an incredibly successful marketplace in Covered California and expanded Medi-Cal for adults. In doing so, California provided more children the chance to have coverage, for when parents are enrolled in health insurance, their kids are more likely to be covered.
But despite the progress we have made, we know there is still more work to do. In 2014, California was home to 323,000 uninsured Latino children—the second largest number of any state in the country. Children without insurance are less likely to get the preventive care they need to stay healthy and more likely to face chronic conditions like diabetes or asthma. With a health insurance card in hand, families can take their children to the doctor and dentist on a regular basis, not just when there is an emergency.
Later this year, California will see an expansion of Medi-Cal to include an estimated 170,000 undocumented children. Our state continues to demonstrate leadership as we work to provide every child access to quality, affordable health coverage. In my new role at The Children’s Partnership, I look forward to working with organizations across the state to help get us to 100 percent insurance rate for our future Latino leaders. When we make sure Latino children are covered and healthy, we ensure the future of California is healthy, too.
- Read the report, Historic Gains in Health Coverage for Hispanic Children in the Affordable Care Act’s First Year.
- Read the press release in response by the Children’s Health Coverage Coalition.
- Share at the infographic below by the Children’s Health Coverage Coalition Coalition.
More than a decade ago, The Children’s Partnership teamed up with small business leaders to connect employees and their families to health coverage. While the portion of uninsured children has reduced since that time, workplaces continue to be an important place to engage families with information about how to get their children enrolled in health coverage. One in three uninsured children in California has a parent working for a small business, and many of them are eligible for no- or low-cost health coverage through Medi-Cal or for financial help through Covered California’s individual marketplace. That is why we have rejoined forces with small business leaders in California to make sure families have what they need to connect to care.
Because of certain provisions in the Affordable Care Act (ACA) that take effect this year, this is a critical time when more people, especially those in the small business community, will be paying attention to the legal landscape of how the ACA impacts small businesses and other employers, including the Employer Shared Responsibility Provision and the Small Business Health Options Program (SHOP). While small businesses—those with 49 or fewer full-time employees—are not required to provide health insurance for their workers, Covered California for Small Business can help many employers withfinancial assistance as well as health insurance options. Small businesses with 25 or fewer full-time employees have the opportunity to receive up to a 50 percent tax credit (35 percent for tax-exempt employers). Employers with 10 or fewer full-time employees qualify for the maximum credit. If they do not offer insurance, employers are encouraged to provide information to employees about affordable health coverage opportunities through Covered California and Medi-Cal. Given the important connection they have to eligible families, small business employers need tools and resources to educate their employees about coverage options for the entire
The Children’s Partnership worked with Small Business California, Small Business Majority, Health Law Guide for Business, The California Endowment, and Covered California to develop resources for small businesses to help their employees and families connect to coverage. Please share our flyer and paycheck envelope stuffer with small businesses in your community and encourage them to distribute information.
When children have health coverage, it benefits children, parents, and employers alike! Studies show that when children have health insurance, their parents are less stressed, miss fewer days of work, and are more productive.
If you act now, you can help connect families to coverage before Covered California’s open enrollment ends on January 31. There are also plenty of opportunities to connect individuals to health coverage year round through Medi-Cal, and eligible individuals can enroll in Covered California anytime if they experience a qualifying life event, such as having a baby, getting married, or moving.
Share this link with small businesses you know in your community: www.childrenspartnership.org/smallbusinessforkidshealth.
Learn more about TCP’s strategy.
Download the flyer for small businesses (English and Spanish).
Download the paycheck envelope stuffer for small businesses (English and Spanish).
Download the briefing document, “Connecting California Children to Health Coverage Through Small Business.”
We are now in the midst of the third open enrollment period for Covered California, the state’s marketplace for affordable health coverage options. And schools and early learning centers across California are once again at the forefront working to inform families about the opportunity to enroll in coverage. Using The Children’s Partnership’sALL IN For Health toolkit, schools and early learning sites are making calls, passing out flyers, sending newsletters, sharing social media messages, and, ultimately, connecting families to enrollment assistance.
But after a successful first two years of enrollment, what should schools and other outreach partners be focused on this year? Based on the research, we know there are some top points to emphasize to make sure kids and their families get covered and stay covered:
- Financial Help Can Lower Monthly Costs: A recent Covered California survey showed that many uninsured individuals who can benefit most from affordable coverage options still do not understand that they can get financial help to lower monthly costs. Therefore, we need to focus our messages on the premium subsidies available through Covered California and the fact that Medi-Cal is free or very low cost. On the flip side, it is also important to remind families that if they don’t get coverage, they might have to pay a fine of $695 per person or 2.5 percent of their income—whichever is greater.
- Enrollment Help Is Available: Studies after previous enrollment periods demonstrate that many people seeking health coverage prefer to talk with someone who can help them understand their coverage options. ALL IN can arrange for Certified Enrollment Counselors who speak English, Spanish, and potentially other languages to be available on site—such as at schools or early learning centers to walk families through the enrollment process and ensure they enroll.
- Shop Around and Renew Every Year: Each year there are new plans and new prices available. Everyone is encouraged to shop the health coverage marketplace during open enrollment and ensure they have the plan that best meets their family’s needs and budget, especially if the family has had any changes in income. For those with coverage through Covered California that are satisfied with their coverage, they will be automatically re-enrolled in their health plan. Medi-Cal will mail renewal packets each year, and families must respond to keep their coverage.
These are just a few messages schools and early learning providers can spread to make this third year of open enrollment as successful as possible. If you have additional ideas on what to focus on or would like to partner with the ALL IN For Health Campaign, please contact us.
Download resources from The ALL IN For Health Fall 2015 Toolkit.
Covered California open enrollment is November 1, 2015, to January 31, 2016. Medi-Cal enrollment is available all year long. Apply through www.coveredca.com.
As we begin the third Covered California open enrollment period, we now have new data to show how well we have done so far in reducing the number of uninsured children in California. The new report, released jointly by Georgetown University Center for Children and Families and the California Children’s Health Coverage Coalition, shows that 176,000 fewer children in California were uninsured in 2014 compared to 2013. That 1.9 percent drop amounts to a statewide uninsurance rate of 5.4 percent compared to 6 percent nationally.
Many of the improvements in children’s coverage rates can be attributed to new coverage opportunities for children through Covered California as well as the Medi-Cal expansion for adults and the continued success of Medi-Cal in meeting the health coverage needs of uninsured children and families. Of note is that the Medi-Cal expansion for parents led to more children enrolling in Medi-Cal coverage, known as the “welcome mat” effect—when parents are eligible for coverage, they are more likely to enroll their eligible children. The increase in coverage is also a result of forward-thinking approaches to simplifying enrollment for eligible individuals. For example, Express Lane Enrollment, a streamlined enrollment process into Medi-Cal for those who are already enrolled in the Supplemental Nutrition Assistance Program (SNAP, formerly the Food Stamp Program), led to hundreds of thousands of adults and children being automatically enrolled in Medi-Cal health coverage because they were enrolled in SNAP.
Committed state leaders are to thank for these great strides in connecting California children and families with the health care opportunities made available by the Affordable Care Act (ACA). At The Children’s Partnership, we’ve also seen education leaders step up and connect students and families to health coverage through our ALL IN For Health Campaign. Through partnerships with education leaders and others, our collective efforts enable us to reach families where they are and connect children to coverage, improving their ability to succeed academically and stay on track developmentally so they can achieve their full potential.
But we still have more to do. California ranks 29th nationally when it comes to kids’ coverage, and there are still about 497,000 uninsured children in California, most eligible for Medi-Cal but not enrolled. This Covered California open enrollment period, and throughout the year for Medi-Cal, we can continue to focus on enrolling these remaining uninsured kids.
We also now have an opportunity to do even more for children in the implementation of Health for All Kids—which will provide Medi-Cal coverage to over 170,000 children who did not previously qualify. Beginning as early as May 1, 2016, all income-eligible children, regardless of immigration status, will be eligible for Medi-Cal. It’s up to us to ensure we make enrollment for these children as smooth and expedient as possible, and TCP will work with the State to help make that happen.
The Children’s Partnership will continue to partner nationally with Georgetown CCF and in California with the Children’s Health Coverage Coalition—which also includes California Coverage and Health Initiatives, Children Now, Children’s Defense Fund-California, PICO California, and United Ways of California—to promote and enhance the Affordable Care Act for kids.
Read the story in Public News Service.
Open enrollment in the state’s health coverage marketplace, Covered California, is available from November 1, 2015–January 31, 2016. Medi-Cal enrollment is available year round. Apply at coveredca.com.
Originally Posted in Say Ahhh! A Children’s Health Policy Blog
By Sonya Schwartz
Now Playing: Coverage for more than 400,000 children and youth
Coming Soon: Coverage for more than 800,000 additional immigrant children, youth and parents
This week, Georgetown University’s Center for Children and Families and The Children’s Partnership released a new paper outlining how to get ready for big coverage opportunities in California. It highlights opportunities that will provide coverage to more than a million people in California’s immigrant families when immigration relief takes affect.
But as spelled out in the paper, Immigration Relief for Parents and Youth = Whole Family Health Coverage in California, while we wait for some of the immigration relief-related coverage options in California to become available, there is a lot that advocates and community organizations in California can do right now to cover eligible children and youth in immigrant families. Here is the run down of coverage opportunities “now playing” in California and also “coming soon” that could get many more children, youth and parents in immigrant families covered.
Now Playing: More than 400,000 children in immigrant families are already eligible for full scope or state-funded Medi-Cal but are not yet enrolled. It is not too soon to roll up our sleeves and get to work on covering them. Here’s the breakdown:
- More than 200,000 youth who qualify for the 2012 DACA program are estimated eligible for Medi-Cal but not yet enrolled. The initial DACA program announced in 2012 is for youth who came to the US before their 16th birthday; have continuously lived in the US since January 15, 2008; are at least 15 years old; are currently enrolled in school or qualifying adult education; or have graduated or obtained a certificate of completion of high school. Our estimates show that of the 343,000 youth qualified for the 2012 DACA program in California, 60 percent or 206,000 are uninsured and eligible for state-funded Medi-Cal. Not all of these 343,000 youth have applied for or been granted DACA status, but if they do receive DACA status and meet the income requirements, they are eligible for a state-funded version of Medi-Cal.
- More than 200,000 citizen or lawfully residing children in immigrant families are eligible for Medi-Cal but not yet enrolled. Our estimates show that 1.6 million children are living with immigrant parents who will be eligible for the new DAPA program in California. DAPA was announced on November 20, 2014, and, when implemented, will allow undocumented immigrant parents who have U.S. citizen or lawful permanent resident children, to apply for work authorization and protection from deportation, if the parent has been in the U.S. since January 1, 2010. Of those 1.6 million California children in DAPA families, 14 percent or 223,000 children are currently eligible for full scope Medi-Cal but remain uninsured. Reaching and enrolling these 223,000 children living in DAPA families would make a huge dent in the number of California’s uninsured children. This map shows that most of these DAPA families live in Southern California with the greatest concentration in Los Angeles County, followed by Orange County, San Diego County, Riverside County, and San Bernardino County.
Coming Soon: There are also opportunities to provide health coverage to more than 800,000 additional immigrant children, youth, and parents and the time to prepare is now. California just passed a law that will provide coverage to all children regardless of immigration status. And, when Deferred Action for Parents of Americans and Lawful Permanent Residents (DAPA) the 2014 expanded Deferred Action for Childhood Arrivals (DACA) program take effect, hundreds of thousands of children, youth, and parents will be eligible for state-funded Medi-Cal. People granted DAPA or DACA statuses are not eligible for federal matching funds for Medicaid or CHIP or for federal premium tax credits in the health insurance marketplace. However, California provides state-funded Medi-Cal coverage for persons residing under color of law (or PRUCOLs), and DACA grantees.
- 170,000 children in California will be eligible for state-funded Medi-Cal for children regardless of immigration status. California recently passed a budget bill (SB 75) that includes health coverage for all children up to 266 percent of the federal poverty level, regardless of immigration status. Children will enroll in a state-funded version of Medi-Cal and coverage will begin no sooner than May 2016. The expansion is estimated to cover 170,000 children.
- More than 600,000 parents in California will qualify for DAPA and likely to be eligible for state-funded Medi-Cal if granted DAPA status. More than 1 million parents in California are estimated to qualify for DAPA and 56 percent are low income by Medi-Cal standards and lack health insurance.
- More than 50,000 youth in California will qualify for the 2014 expanded DACA program and are likely to be eligible for state-funded Medi-Cal if granted DACA status. The expanded DACA program, announced on November 20, 2014, but on hold because of litigation, is also for youth who came to the US before their 16th birthday but who have continuously lived in the US since January 1, 2010 and meet other requirements. Estimates show that of 92,000 youth qualified for expanded DACA, 60 percent or 55,200 are uninsured and likely eligible for state-funded Medi-Cal.
If you are a children’s or immigration advocate or social service provider in California, our paper also provides specific suggestions about what you or your organization can do to help get children, youth, and parents in immigrant families covered. If advocates, service providers, and others working on health care, immigration, and child and family well-being work together to educate and enroll children and families in health insurance, it could lead to a significant reduction in California’s uninsured rate.
State-funded Medicaid coverage for DAPA and DACA grantees and the new coverage opportunity for children regardless of immigration status is unique to California and a few other states. But, all states cover citizen children in immigrant families. And, the majority of other states (twenty-eight) provide coverage to lawfully residing children in immigrant families. Although, there is always more work to be done get these eligible children enrolled in health coverage.
Continue reading on the Georgetown Center for Children and Families website.
Today marks 50 years since Medicaid was signed into law and it is truly a day to celebrate. The program has had a long, successful history of bringing health care to children and families most in need. A combined federal-state effort to finance health programs and ensure timely care, Medicaid provides coverage for nearly 33 million children, or 37 percent of all children living in the United States. All of these children are able to get regular preventive care, from well-child visits and immunizations to dental, hearing, and vision care. And Medicaid provides services for children with special health care needs as well.
Now that longitudinal data is available, we can squarely say that the benefits of providing health care go far beyond the doctor’s office. In honor of the occasion, our partners at The Georgetown Center for Children and Families released a report detailing the growing body of research that shows the long-term benefits Medicaid has provided to children and the nation. Children with access to Medicaid are proven to have better health as adults, with one study showing a 26 percentage point decline in the incidence of high blood pressure in adulthood. Enrollment in the program is also associated with greater academic achievement and higher likelihood of graduating from high school and college. And recent studies suggest that giving low-income kids access to health coverage boosts their future earnings for decades, therefore increasing their future income tax contributions and helping generate an even bigger return on investment.
California is leading the way in giving families peace of mind, knowing that their children have health coverage that allows them to be healthy and productive. Thanks to recent action, starting no sooner than May 2016, California will cover the last remaining group of uninsured children—those who are undocumented. This will ensure more kids in the state than ever before can get a fair shot in life and will help reduce California’s still-unacceptable 7.4 percent children’s uninsurance rate in the state.
In California, and across the nation, we need to continue to both protect and expand Medicaid. The benefits to children’s health, education, and long-term prosperity could not be clearer. On the fiftieth anniversary, let’s commit to keeping Medicaid strong for future generations of children.
In 1997, The Children’s Partnership joined with a small group of children’s advocates and supporters and set an audacious goal—securing health coverage for every child in California. With a name that was aspirational, accountable, and determined, we called our effort the “100% Campaign.”
When our journey began, California had nine million children, and 1.74 million of them (nearly one in five) had no health insurance. The reasons varied from lack of affordable coverage options, to a 28-page application form, to policies that precluded eligibility for most immigrant children.
During this time, the Clinton Administration’s effort to enact health care for all Americans was blocked, and the bipartisan Children’s Health Insurance Program (CHIP) emerged to address the needs of children whose families make too much money to be covered by Medicaid, but cannot afford private insurance. Meanwhile, California was battling a voter-passed initiative (Proposition 187) in the courts that would have denied most public benefits to immigrants without documentation. At this juncture, our campaign knew there would be an uphill climb to this goal.
The 18-year trek included numerous efforts and hard-won, step-by-step progress—a testament to the persistent, at times creative and at times heroic efforts of policymakers and their staff, foundations who stayed the course, health providers, community organizers, and consumer advocates. Beginning in 2001 with a local pilot in Santa Clara County that demonstrated the health and cost benefits of covering all kids, local Children’s Health Initiatives were expanded over time to become available to children in 30 of California’s 58 counties at their peak. A dedicated group of California leaders tried most every tack possible, including a state legislative and budget effort, a tobacco tax measure on the 2006 ballot, and an attempt by Governor Schwarzenegger to enact state health reform. But budget setbacks, tobacco industry opponents, and legislative opponents frustrated the progress.
Amidst these attempts that came close to covering all kids but failed, impressive progress was made over the years. The Healthy Families Program—California’s CHIP—grew to provide subsidized coverage to hundreds of thousands of children in working families; the 28-page application form was replaced by a far shorter one; and Express Lane Eligibility made it easier to enroll large numbers of uninsured children already certified for other income-tested programs like the National School Lunch Program in health coverage programs. The passage of the landmark Affordable Care Act in 2010 opened up coverage options to many more families, but still the job was not complete.
Even with setbacks, we were not defeated, our resolve strengthened with the knowledge that the public was in favor of coverage for all kids, including undocumented immigrants.In 2005, four out of five voters (78 percent) supported a statewide plan to “ensure that every child in California has health insurance,” with more than half (55 percent) saying they “strongly support” it. In 2014, a majority supported expanding existing health care programs to cover all low-income Californians, regardless of immigration status.
After nearly two decades, policymakers’ actions caught up with public support. Last week, a historic budget was signed by Governor Jerry Brown extending health benefits to undocumented children. Now, we can finally say the original goal of securing coverage for 100 percent of California’s children is a practical reality.
Any good advocate will point out that the job isn’t finished as we work to implement these changes and actually enroll children, and to be sure that securing health coverage translates into meaningful access to health care and improved health for children. In addition, it is time for policymakers to step up and support offering affordable coverage for family members as well as children.
But, it is just as important to herald this moment and acknowledge the work of our state leaders and countless others to achieve a goal so important and so right as making sure that every child in the Golden State has a chance to grow up healthy. It is a 100 percent great moment for California and our kids.
- « Previous
- 1
- 2
- 3
- Next »